SASH introduced the Let’s Get You Home initiative to ensure patients spend no longer than they need to in hospital on 17 April.
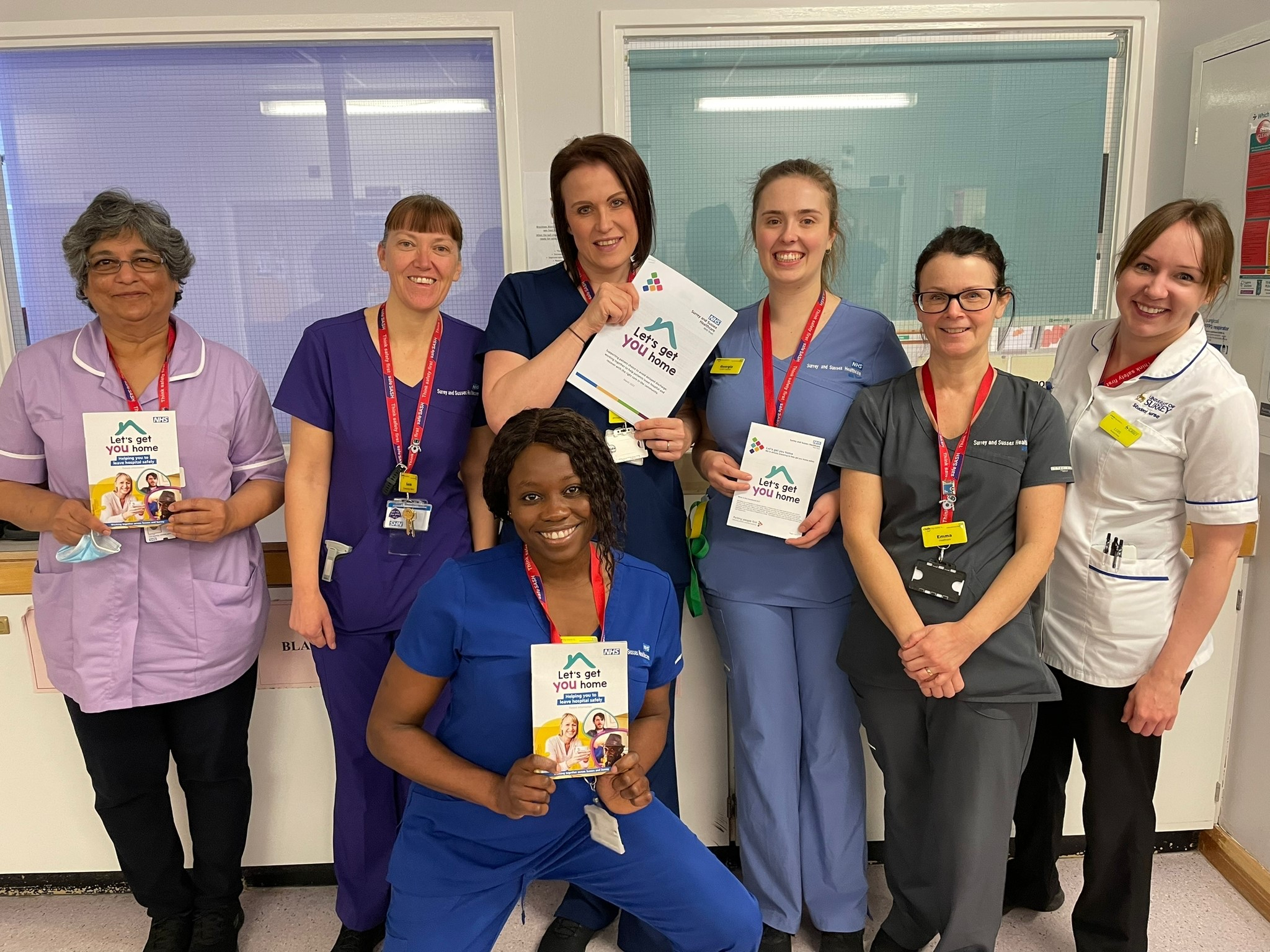
Katie Davies, acting ward manager and gynaecology outpatients nurse manager on Brockham ward and Aldrich Blake unit shares how the team have adopted the Let’s Get You Home policy to support timely discharge.
Katie said: “We’ve been focussed on timely discharge, so the introduction of the Let’s Get You Home initiative wasn’t something new, but it has really helped us remove any obstacles in the way of appropriate discharge. We already have updated daily targeted discharge dates and criteria to reside, but the policy has formalised this.”
Since the initiative was introduced, the team have been talking to all patients that come in about their targeted discharge date.
Katie said: “All patients are given the Let’s Get You home patient information leaflet explaining the discharge process and a target discharge date on admission. It all really comes down to clear communication at the start of a patient’s care journey.
“For example, there was a lady on our ward and straightaway we explained when we’d expect her to be discharged, helping to manage her expectations. It worked really well.”
Each week, Katie puts a reminder message on the back of handover documents, ranging from clinical updates to the SASH Star of the Month award, and last week, the focus was on the Let’s Get You Home initiative.
“It’s an easy and effective way to make sure staff are aware of the policy and are embedding it into their everyday practice. It really does encourage discussion among the team.”
The Let’s Get You Home policy clearly outlines the escalation processes to follow when staff have a challenging discharge.
Katie said: “For example, recently we had a patient transferred to us from Copthorne ward. This patient has been with us for 48 days. We automatically start asking the questions; ‘why haven’t they been transferred’ and ‘what’s holding up the discharge?’ We rang the community matrons to see is this patient could be moved to a community bed, because this patient had been medically fit for some time. The patient wasn’t keen to move.
“Yesterday, the matron and I talked to this patient about her discharge, explaining why an acute hospital wasn’t the environment for her, using the policy to guide us. We managed to get to the reason why she wouldn’t leave and got her to change her mind.”
The team have been planning discharges by ensuring discharge summaries and TTOs are ready as well as utilising the discharge lounge.
“We’ve had to adapt how we do our ward rounds because of the different disciplines on the ward” says Katie “but the policy has given staff more confidence. It all comes down to teamwork. If we’re in agreement that a patient is medically fit to be discharged, we’ll have those conversations, using the Let’s Get You Home policy to support us.”
Katie produces a monthly newsletter for the team and May’s edition will focus on timely discharging using the policy and encouraging staff to read and use it. She has now expanded on the progress on documenting the standards of care by introducing an admission slip, following a dig into why there was failure in their nursing documentation audit. The new slip, which has a list of actions, including running through targeted discharge dates, has to be completed with every admission.
“This is particularly helpful when, for example, patients come in overnight and certain assessments are not noted down” says Katie. “Now the slip goes hand in hand with the Let’s Get You Home patient leaflet, and if any section is left incomplete, it is handed over to the next shift.”
Since the team have embedded best practice with the use of criteria to reside and targeted discharge dates, and the use of the patient information leaflet, Katie has seen improvement.
She said: “We’ve had positive feedback from patients and it’s great to see staff working together to improve outcomes.”
