Screening tests for you and your baby (EN hardcoded) from NHS Screening on Vimeo.
Screening tests for you and your baby (EN) from NHS Screening on Vimeo. For translated version, click here.
For information on screening tests for you and your baby in multiple languages, please click here. You can also read more here.
SASH Maternity Services will offer you a number of screening and diagnostic tests during your pregnancy. Your midwife will advise you which tests are offered and why. These tests can help you find out about your own health and the health of your baby before birth.
All of the tests are optional – it’s your choice whether to have the test or not. The information these tests can provide will help you make choices about your pregnancy, and help your midwife and doctor to provide the best care possible for you and your baby during your pregnancy, the birth and once baby has been born.
You will be asked to consent to the test with information shared face-to-face at each appointment.
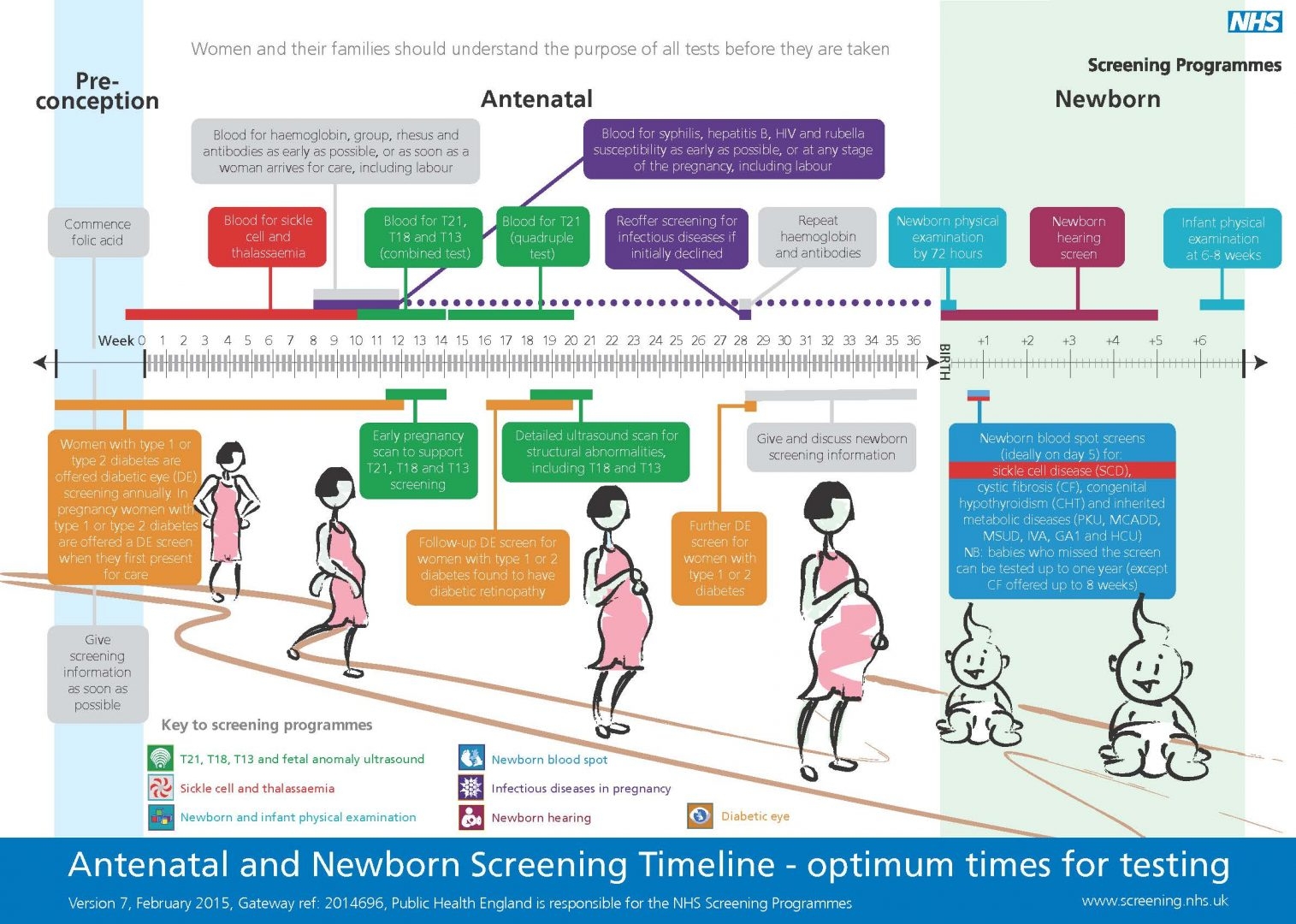
The diagram below explains what tests will be performed, and at which stage of the pregnancy: